53 YR OLD MALE WITH FEVER SINCE 4 DAYS
18/1/2023
Roll.no :51
"This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome."
" I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan "
53 YR OLD MALE WITH FEVER AND ABDOMINAL DISCOMFORT SINCE 4 DAYS
A 53 yr old male came to OPD with
Chief complaints of :
- fever since 4 days
- abdominal discomfort , bloating and loss of appetite since 4 days
- burning micturition since 4 days
- no passage of stools since 4 days
HISTORY OF PRESENT ILLNESS :
- Patient was apparently asymptomatic 4 days back , he then developed fever , high grade , intermittent in nature , associated with chills and rigors , headache ,no diurnal variation , relieved by medication
- patient complains of burning micturition since 4 days .
- H/O loss of appetite since 4 days .
- the patient complains of abdominal discomfort and bloating after having food
- H/O unable to pass stools since 4 days
- H/O SOB +
- No H/O vomiting , cough , cold , pedal oedema
DAILY ROUTINE :
patient wakes up at 4:30 am in the morning and goes to work
- he works as a farmer and does wood cutting
- he has tea everyday at 7 am on empty stomach and his breakfast is usually rice with some curry at 11:00 am
- he has lunch at 1:30 pm which is rice or dosa
- he returns back from worn at 6:00 pm , watches tv and has dinner around 8 pm which is usually rice and curry
- he sleeps by 10 pm
PAST HISTORY :
K/C/O DM 2 since 10 yrs , on regular medication ( Metformin 500 mg + Glimiperide 1 mg )
Surgical history :-
- K/C/O CAD - PTCA done 4 yrs back , 1 stent placed
- patient underwent appendicectomy in in 2015
- hydrocele surgery ( left jaboulay's procedure ) done in 2017
- lumbar spine fixation surgery done in 2016 and rods placed
- Not a k /c/ o HTN , Thyroid , TB , Asthma Epilepsy , CVA .
Family history : not significant .
PERSONAL HISTORY :
Diet - mixed
Appetite - reduced since 4 days
Bowel movements - constipation since 4 days , bladder - regular
Sleep - adequate
Addictions : consumes alcohol regularly since 20 yrs , 90 ml / day
- stopped smoking 4 yrs back , patient used to smoke 2 packs of cigarettes daily for 25 y rs
- No allergies
GENERAL EXAMINATION :
- Patient was examined after taking his consent
- Patient is conscious , coherent , cooperative , well oriented to time , place and person .He is moderately built and nourished
- No signs of pallor , icterus , cyanosis , clubbing , oedema , lymphadenopathy .
His vitals:
Temperature : 99.6 F
BP : 120/80 mm HG
Pulse rate : 78 / min
Resp.rate : 16 cpm
GRBS : 167 mg/dl
Spo2 : 98 percent
Systemic Examination:
CVS- S1 S2 heard,no murmurs present.
RS - bilateral Air entry present
Normal vesicular breath sounds heard
Per Abdomen : soft , tenderness + in epigastrium and right hypochondrium , bowel sounds + , no signs of organomegaly
CNS :higher mental functions : normal
Reflexes :
MOTOR-: normal tone and power
reflexes:
RT L T
Biceps ++ ++
Triceps ++ ++
Supinator ++ ++
Knee ++ ++
Ankle ++ ++
Investigations:
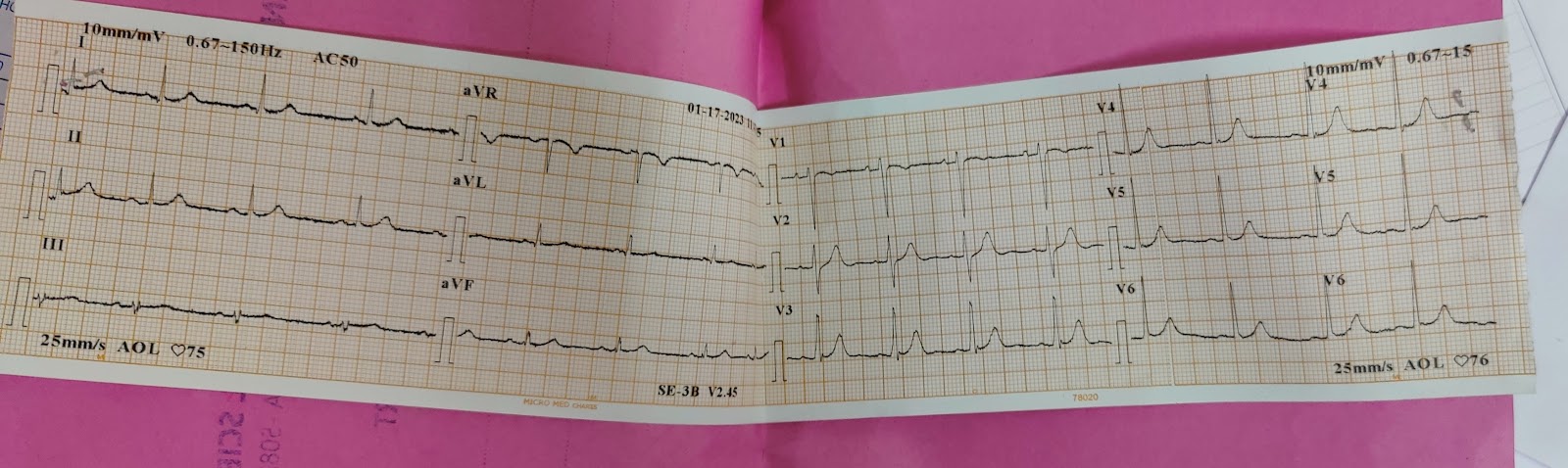
ECG
2 D echo
Chest XRay PA view
Xray erect abdomen
Hemogram
Complete urine examination :
Liver function test
Serology : HBSAg : negative , HIV : negative , HCV : negative
USG Abdomen :
I/v/O right renal calculus , patient advised to take plenty of oral fluids and syp . Alkastone 15 ml / bd
Provisional diagnosis:
Viral pyrexia with thrombocytopenia with HFPEF with RHF
Treatment :
1 inj pan 40 mg IV/OD
2 Inj vit b complex with vit b12 , 1 amp in 100 ml NS IV / OD
3. Inj . thiamine 200 mg in 100 ml NS IV/ BD
4.inj furosemide 40 mg IV/ BD
5.tab PCM 650 mg TID
6 inj h. Actrapid insulin sc/ tid , inj nph insulin sc/ bd
7 . Syp cremaffin PO / HS
8 syp.potklor 15 ml PO/ TID
9. High fibre diet
10 . Oral fluids upto 1.5 lit / day.
11. 1 amp KCL in 1 pint NS over 6 hrs
12 . GRBS monitoring 7 pint profile
13 . Vital monitoring 4 th hrly
On 19/1/23
- C/ O bilious vomiting ( 1 episode )
- 4 fever spikes in the night , 3 stools passed
-Patient is conscious , coherent , cooperative , well oriented to time , place and person
His vitals:
Temperature : 99.6 F
BP : 120/80 mm HG
Pulse rate : 82 / min
Resp.rate : 19 cpm
GRBS : 115 mg/dl
Spo2 : 98 percent
I/O : 1800/650 ml
CVS : S 1 , S 2 heard
RS : BAE + , NVBS +
P/A : soft , non tender , BS +
CNS : NFND
A : Viral pyrexia with thrombocytopenia with HFPEF with RHF
Management :
inj pan 40 mg IV/OD
2 Inj vit b complex with but b12 1 amp in 100 ml NS IV / OD
3. Inj . thiamine 200 mg in 100 ml NS IV/ BD
4.inj furosemide 40 mg IV/ BD
5.tab PCM 650 mg TID
6 inj h. Actrapid insulin sc/ tid , inj nph insulin sc/ bd
7 . Syp cremaffin PO / HS
8 syp.potklor 15 ml PO/ TID
9. High fibre diet
10 . Oral fluids upto 1.5 lit / day.
11. 1 amp KCL in 1 pint NS over 6 hrs
12 . GRBS monitoring 7 pint profile
13 . Vital monitoring 4 th hrly
20/1/2023
AMC
Bed 1
Day 3
S : vomitings bilious ( 2 episodes )
No fever spikes
Diffuse pain abdomen
loose stools ( episodes 4 )
O :
Patient is conscious , coherent , cooperative , well oriented to time , place and person
His vitals:
Temperature : 99.6 F
BP : 120/80 mm HG
Pulse rate : 82 / min
Resp.rate : 20 cpm
GRBS : 125 mg/dl
Spo2 : 98 percent
I/O : 2000/950 ml
CVS : S 1 , S 2 heard
RS : BAE + , NVBS +
P/A : soft , non tender , BS +
CNS : NFND
A :
Viral pyrexia with thrombocytopenia with HFPEF with RHF , wet beri beri , old CAD , ? Alcoholic gastritis
P :
1 inj pan 40 mg IV/OD
2 Inj vit b complex with but b12 1 amp in 100 ml NS IV / OD
3. Inj . thiamine 200 mg in 100 ml NS IV/ BD
4.inj furosemide 40 mg IV/ BD
5.tab PCM 650 mg TID
6 inj h. Actrapid insulin sc/ tid , inj nph insulin sc/ bd
7 . Syp cremaffin PO / HS
8 syp.potklor 15 ml PO/ TID
9. High fibre diet
10 . Oral fluids upto 1.5 lit / day.
11. 1 amp KCL in 1 pint NS over 6 hrs
12 . GRBS monitoring 7 pint profile
13 . Vital monitoring 4 th hrly
21/1/23
S : C/O headache , no fever spikes
O :
Patient is conscious , coherent , cooperative , well oriented to time , place and person
His vitals:
Temperature : 98.6 F
BP : 120/80 mm HG
Pulse rate : 92 / min
Resp.rate : 18 cpm
GRBS : 132 mg/dl
Spo2 : 99 percent
I/O : 450/750 ml
CVS : S 1 , S 2 heard
RS : BAE + , NVBS +
P/A : soft , non tender , BS +
CNS : NFND
A :
Viral pyrexia with thrombocytopenia with HFPEF with RHF , wet beri beri , old CAD , ? Alcoholic gastritis
P :
1 inj pan 40 mg IV/OD
2 Inj vit b complex with but b12 1 amp in 100 ml NS IV / OD
3. Inj . thiamine 200 mg in 100 ml NS IV/ BD
4.inj furosemide 40 mg IV/ BD
5.tab PCM 650 mg TID
6 inj h. Actrapid insulin sc/ tid , inj nph insulin sc/ bd
7 . Syp cremaffin PO / HS
8 syp.potklor 15 ml PO/ TID
9. High fibre diet
10 . Oral fluids upto 1.5 lit / day.
11. 1 amp KCL in 1 pint NS over 6 hrs
12 . GRBS monitoring 7 pint profile
13 . Vital monitoring 4 th hrly
Investigations :
Blood urea : 43
Creatinine : 1.0
Na : 128
K : 3.9
Cl :98
22/1/23
S :
Stools not passed since yesterday
Blurring of vision since 1 day
O :
Pt is conscious , coherent cooperative
His vitals:
Temperature : 98.6 F
BP : 120/80 mm HG
Pulse rate : 92 / min
Resp.rate : 18 cpm
GRBS : 175 mg/dl
Spo2 : 99 percent at RA
I/O : 450/750 ml
CVS : S 1 , S 2 heard
RS : BAE + , NVBS +
P/A : soft , non tender , BS +
CNS : NFND
A :
Viral pyrexia with thrombocytopenia with HFPEF with RHF , wet beri beri , old CAD , ? Alcoholic gastritis , peripheral neuropathy secondary to DM / Alcohol
P :
inj pan 40 mg IV/OD
inj furosemide 40 mg IV/ BD
tab PCM 650 mg SOS
inj h. Actrapid insulin sc/ tid
Tab pryoboi 75 mg PO / HS
Tab ECOSPRIN AV 75/10 HS
Tab benfomet plus PO/BD
High fibre diet
Oral fluids upto 1.5 lit / day with ORS sachets in 1 litre water
GRBS monitoring 7 pint profile
Vital monitoring 4 th hrly
23/1/23
S :
C/O swelling of both lower limbs
O :
O :
Pt is conscious , coherent cooperative
His vitals:
Temperature : 97.6 F
BP : 110/80 mm HG
Pulse rate : 94 / min
Resp.rate : 18 cpm
GRBS : 175 mg/dl
Spo2 : 99 percent at RA
I/O : 450/750 ml
CVS : S 1 , S 2 heard
RS : BAE + , NVBS +
P/A : soft , non tender , BS +
CNS : NFND
A :
Viral pyrexia with thrombocytopenia ( resolved ) with HFPEF with RHF , wet beri beri , old CAD , ? Alcoholic gastritis , peripheral neuropathy secondary to DM / Alcohol
P :
tab PCM 650 mg SOS
inj h. Actrapid insulin sc/ tid
Tab pryoboi 75 mg PO / HS
Tab ECOSPRIN AV 75/10 HS
High fibre diet
Oral fluids upto 1.5 lit / day with ORS sachets in 1 litre water
GRBS monitoring 7 pint profile
Vital monitoring 4 th hrly





















Comments
Post a Comment